VA Philadelphia health care
At the VA Philadelphia Healthcare System, our expert health care teams focus on your needs and the needs of other Veterans, your families, and caregivers. Find a health care facility near you, and manage your health online. Sign up for community events and updates, and learn what’s new at your local VA medical center and clinics.
Locations
Corporal Michael J. Crescenz Department of Veterans Affairs Medical Center

Manage your health online
In the spotlight at VA Philadelphia health care
Stories
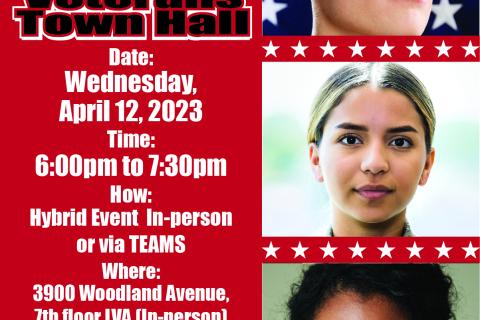
2023 Women Veterans Town Hall recap and resources
The Corporal Michael J. Crescenz VA Medical Center (CMCVAMC) hosted a Women Veterans Town Hall on April 12, 2023. The event featured remarks from the Medical Center Director, VBA Executive Director, , and Guest Speakers from Fox Chase Cancer officials from the VBA and NCA..
Historic Public-Private partnership between the VA and University of Pennsylvania Health System (UPHS)
History was made on June 27th as a momentous public-private partnership was announced and commemorated through the signing of a Memorandum of Understanding (MOU) between the U.S. Department of Veterans Affairs Veterans Health Administration (VHA) and the University of Pennsylvania Health System.


